Managing Type 1 diabetes in winter presents unique challenges, such as changes in physical activity, temperature fluctuations, and potentially altering insulin needs. Participating in I Challenge Diabetes programs can be incredibly beneficial for learning how to adapt to these seasonal shifts and stay on top of your diabetes management. Here are some key strategies for managing Type 1 diabetes during the winter months:
1. Monitor Blood Sugar Regularly
- Winter Activity Changes: In colder weather, you might be less active, which can affect your insulin needs. People often tend to be less physically active in winter, which might require adjustments to insulin doses.
- Cold Weather Effects: Cold weather can also cause blood vessels to constrict, which might affect blood sugar readings and insulin absorption. Regular testing helps to catch any fluctuations early.
2. Adjust Insulin Doses
- Reduced Activity: If you’re less active, you might need less insulin, as exercise helps to lower blood sugar levels. Keep track of changes in your activity levels and consult your healthcare provider about adjusting your insulin regimen.
- Insulin Sensitivity: Some people experience changes in insulin sensitivity during winter months, so it’s important to monitor how your body responds to insulin and make necessary adjustments.
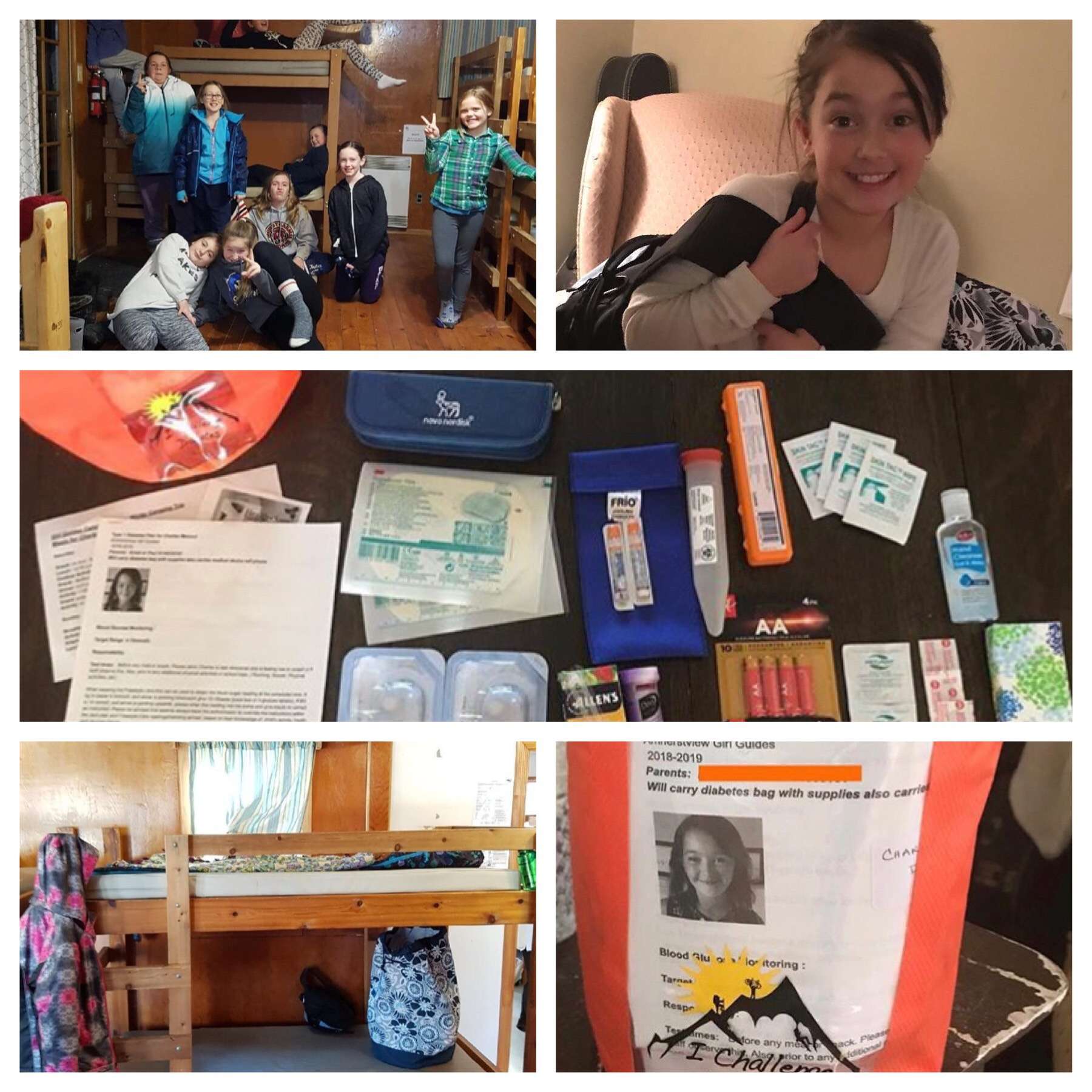
3. Keep Insulin and Supplies Warm
- Avoid Freezing: Insulin should be kept at room temperature and away from freezing conditions. Cold temperatures can cause insulin to lose its effectiveness.
- Proper Storage: Always store your insulin in an insulated bag, especially if you’re spending time outside in freezing temperatures.
4. Stay Active, but Safely
- Winter Sports: Activities like skiing, snowboarding, or ice skating can be great ways to stay active, but they may cause blood sugar to drop quickly. Be sure to carry fast-acting carbs with you, and test your blood sugar before, during, and after activity.
- Indoor Exercise: If outdoor activities aren’t possible, try indoor workouts to maintain your fitness level. Activities like yoga, Pilates, or even indoor cycling can help keep your blood sugars stable.
5. Eat a Balanced Diet with Seasonal Foods
- Healthy Comfort Foods: Winter often brings hearty meals like stews, soups, and roasts. Opt for nutrient-dense meals that are high in fiber and balanced with protein, healthy fats, and low glycemic carbohydrates.
- Carb Counting: Since comfort foods tend to have higher carb content, it’s important to count carbs carefully to avoid blood sugar spikes.
- Winter Superfoods: Incorporate seasonal foods like root vegetables, leafy greens, and citrus fruits for added vitamins and nutrients.
6. Stay Hydrated
- Dry Air: Winter air tends to be dry, which can lead to dehydration. Dehydration can cause blood sugar to rise, so drink plenty of water throughout the day. Herbal teas or water with lemon can also be refreshing alternatives.
7. Be Mindful of Illnesses
- Flu Season: Winter months often come with an increase in colds and flu. Illness can impact blood sugar levels and insulin needs, so it’s important to stay vigilant with your blood sugar management.
- Get Vaccinated: Ensure you’re up to date with flu and pneumonia vaccines to help reduce the risk of illness.
8. Psychological Well-Being
- Seasonal Affective Disorder (SAD): The lack of sunlight in the winter months can lead to feelings of depression or low energy. These can sometimes make diabetes management more challenging. Participating in I Challenge Diabetes programs can provide emotional support, help keep motivation high, and encourage a sense of community, which is crucial for long-term management.
- Mindfulness and Stress Management: Stress, whether from seasonal changes or daily challenges, can affect blood sugar levels. Consider practicing relaxation techniques like deep breathing, meditation, or mindfulness exercises.
9. Attend I Challenge Diabetes Programs
- Community Support: I Challenge Diabetes offers fantastic resources for both emotional and physical management. Through education, workshops, and group activities, participants can gain better insights into how to manage their diabetes during the winter months, stay motivated, and connect with others who understand the challenges.
- Event-Based Learning: ICD hosts winter-focused events that specifically cover managing diabetes during colder months. I Challenge Diabetes offers support that integrates both lifestyle and health education.
10. Layer Clothing Properly
- Avoiding Hypothermia or Frostbite: Ensure you’re dressing warmly when going outside. Insulin pumps and devices can be sensitive to temperature, so make sure they are kept in a pocket close to your body to prevent them from freezing.
- Foot Care: Pay extra attention to your feet in cold weather. The skin can dry out and crack, increasing the risk of infections. Proper footwear and moisturizers can help prevent foot complications.
By utilizing these strategies, and with the support of I Challenge Diabetes programs, you can successfully navigate winter with Type 1 diabetes. It’s all about staying proactive, adjusting your routine, and seeking the right support system.