3,906 Days & Counting: My Journey with T1D and Parenthood
In June of 2009, my life changed.
A trip to the doctor corroborated the test results we received at home. Pregnant.
As the doctor explained why this was a high-risk situation, and she was not comfortable navigating the pregnancy with us and would be sending us to an Endocrinologist specializing in pregnancy, my husband was brimming. He had always wanted to be a father.
I, however, kept picturing that scene in Steel Magnolias. You know the one. The character portrayed by Julia Roberts, with Type 1 Diabetes, unconscious in the kitchen. Pots boiling over. Baby screaming alone on the floor.
There were several reasons I did not want to have children and an equal number of reasons why I was told having them would be either incredibly difficult or impossible.
Full disclosure: I did not want to burden a child with my chronic illnesses (both mental and physical), nor did I think I would be particularly good at the whole parenting gig.
The news of a successful pregnancy was very unexpected.
My T1D and Pregnancy
I knew nothing of pregnancy and Type 1 Diabetes. The endo and nurse explained little beyond emphasizing the need for tight control.
Pregnancy did not agree with me. I never acquired that pregnancy glow. Nor was it a joyous period in my life. In truth, I only have one picture.
It was riddled with weekly appointments at the high-risk clinic peppered with extra tests, procedures, and specialist visits. Not to forget to mention pricking my finger every 2 hours (including through the night!) and recording the data on a chart for my endo.
I gained almost one hundred pounds over the course of those eight months. And that severely impacted my mental health (I struggle with body dysmorphia).
However, there were some positives.
After living with T1D for a decade, I finally learned how to properly inject myself (and in a pregnant belly) and I finally got to inject an orange (an odd rite of passage in the diabetes realm). My HbA1c was the best it had ever been, remaining around 6% the entire time. And I learned about correction doses, for the first time.
My pregnancy was mostly problem free, save a wee scare in my second trimester and a premature birth.
The weight gain also impacted my physical health and caused me a great deal of pain. All that extra weight placed a lot of pressure on my hips and resulted in one becoming displaced during delivery, which made things incredibly difficult upon arrival home with a newborn.
Early Years
That scene from Steel Magnolias plagued my entire pregnancy and stained the first few years of parenthood.
Our son never went to daycare or preschool. I was his primary caregiver and often allowed my blood sugars to coast out of range for fear of going low while home alone with him.
As a new mom, I was tremendously overwhelmed. My hopes of breast feeding were almost immediately dashed as no one had ever properly explained the impacts of T1D. In the hospital we had to supplement with formula because they were having a hard time getting baby’s blood glucose to stabilize.
I felt guilty, ill-equipped, and like a failure.
Some of those feelings were alleviated when it was discovered our son had a milk allergy and had to be switched to soy formula at the age of five months. Later, on my own, I learned about issues for T1D mothers, like delayed lactation and increased hypoglycaemia.
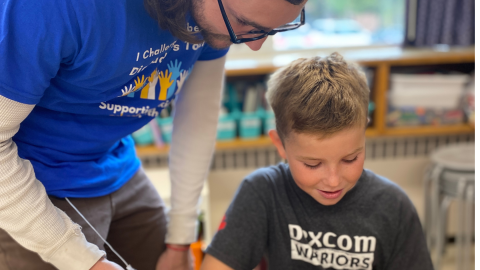
As soon as it could be contextualized, we taught our son about Type 1 Diabetes and showed him how he could help Mommy. By 18 months he was able to assist me in testing my blood sugars and/or grab me a treatment for a low.
Regardless, I kept those sugars high. There would be no hypos on my watch. I never corrected the highs (fear of going low and needle phobia saw to that) and was often emotional.
Those early years were unnecessarily difficult, but also extremely rewarding.
Moving On
It is funny what motivates us.
My own health was never been much of a factor. But the health of the baby inside of me was paramount, so my diabetes management benefited from my pregnancy.
After his birth, I settled into the role of mom and seldom thought of my diabetes. I certainly did not do a particularly good job of managing. I drifted along day in and day out for years with an HbA1c hovering in the double-digits.
My son became increasingly interested in T1D. He was always ready with a hug after a needle phobia induced anxiety attack (something that happened with nearly every injection). He knew what to do if he ever found me unconscious, including calling 911 and administering glucagon.
And he was always eager to learn about our famous cousin Banting, who co-discovered insulin. The very thing that was keeping me alive.
Once I wore a CGM for a week. A free trial offered by my then clinic. He was fascinated and loved being able to look at my blood sugars without me pricking my finger. Unfortunately, at the time, it was financially out of reach for us.
Then he learned about an insulin pump.
For years I had put it off, I did not want something attached to me. I had no desire to make my invisible illness visible. But his tiny little 5-year-old voice chirped, “if it could help you shouldn’t you have it?” Raised eyebrows and some encouragement from my husband solidified his argument.
So, next thing I knew, I was enrolled in the classes necessary when pursuing insulin pump funding here in Ontario. I was one HbA1c and a decision (which pump I wanted) away from receiving it when all was derailed by a cancer diagnosis.
When that was all sorted (two surgeries later), I simply carried on and forgot all about the pump.
Full Circle
As technology became easier to access, I saw improvements in my diabetes management. We added an FGM to my arsenal. My son loved the idea of scanning to see where I was, and then dictating the next step.
By now we had moved, to a new city, and I was at a new diabetes clinic. Both he and my husband gently pushed the idea of re-visiting an insulin pump. So, I did.
While I wish I could say that pursuit was for me, because it should have been, it was not. I did it for my son. I did it because he needs his mom healthy and this was going to help make that happen. I did it because he needs a good example of caring for one’s self (even if the reasons behind it are muddled).
Now, I have two robot parts. I am Cyborg Mom. And my son can and does actively assist in my management.
He has memorized all my CGM alerts. He knows which ones are high, low, and dangerously low. He now knows (and feels much more comfortable) how to administer nasal glucagon. He also knows how to navigate my pump’s PDM and can input blood glucose levels to bolus or run a temp basal or suspend if my hands are otherwise occupied (like driving, gardening, or cooking).
Pregnancy and parenting are not easy roads. Traveling along them with any chronic condition, like Type 1 Diabetes, presents a unique set of challenges. But it is no less rewarding.
And informing those around you, including your child(ren), can potentially save your life.
In the very least, it will change it. For the better.
By Rebecca Redmond

A passionate creative type, Rebecca brings attention to living with Type 1 Diabetes and mental illness to light through writing, speaking, and art. Her desire to raise awareness finds her advocating on a global scale, as she strives to change perceptions of what is “normal” and erase stigma for those living with mental illness, while her family connection to Sir Frederick Banting drives her advocacy in the T1D community.
Find Rebecca on instagram @rebaredmond and @deadpancreasanxiety
FB Rebecca Redmond or Dead Pancreas Anxiety
Twitter @RebaRedmond
Site www.deadpancreasanxiety.com